Cesarean Delivery: Preparing for Surgery & Recovery – Kienthucsannhi.com. In today’s article, kienthucsannhi.com will explore with you in the most detailed and complete way. See now!
Understanding Cesarean Delivery and What to Expect
A cesarean delivery, or C-section, is a surgical procedure that involves delivering a baby through an incision in the mother’s abdomen. This procedure might be planned or unplanned, with reasons ranging from complications during labor to a previous C-section.
What is a Cesarean Delivery?
While many women dream of a natural vaginal birth, sometimes a Cesarean delivery is the safest option for both mother and baby. It’s crucial to understand the reasons behind this decision. You might need a Cesarean delivery for various reasons, such as:
- Premature labor: When a baby is born before 37 weeks of gestation.
- Breech presentation: When the baby is positioned feet or buttocks first instead of head first.
- Placental abruption: When the placenta detaches from the uterine wall before delivery.
- Placenta previa: When the placenta is positioned low in the uterus, blocking the cervix.
- Multiple births: When carrying twins, triplets, or more.
- Fetal distress: When the baby shows signs of distress during labor.
- Prior C-section: If you’ve had a previous Cesarean delivery, your doctor might recommend a C-section for future deliveries.
The Cesarean Delivery Process
During a Cesarean delivery, the medical team will administer anesthesia to ensure the mother feels no pain. The type of anesthesia often used is either a spinal block or an epidural. Then, a surgical incision is made in the abdomen, and the baby is carefully delivered through the incision. The procedure typically takes about 30-60 minutes, but recovery time can vary.
Potential Risks and Complications
While Cesarean deliveries are generally safe, it’s important to be aware of potential risks and complications. These can include:
- Infection: As with any surgical procedure, there is a risk of infection, particularly at the surgical site.
- Bleeding: Heavy bleeding can occur after a Cesarean delivery, requiring blood transfusions in some cases.
- Blood clots: There is a risk of blood clots forming in the legs after surgery.
- Urinary tract infection (UTI): UTIs are a common complication after surgery.
- Wound healing complications: While most incisions heal well, some women may experience wound healing complications, such as infection or delayed healing.
It’s important to remember that these complications are relatively rare, and most women recover fully from Cesarean deliveries. By understanding the potential risks, you can be better prepared to discuss any concerns with your doctor.

Preparing Your Body for Surgery and Recovery
Preparing your body for a Cesarean delivery and recovery is crucial. It involves more than just physical preparation; it’s also about creating the right mental and emotional mindset.
Pre-Surgery Preparation
Before the surgery, your doctor will guide you on how to prepare, including:
- Fasting: You’ll likely be required to fast for a specific period before surgery, depending on the anesthesia type.
- Bowel preparation: Your doctor might recommend a bowel preparation to empty your bowels before surgery, making the procedure easier.
- Blood tests: You will likely have blood tests to check your blood type and hemoglobin levels.
- Fetal monitoring: Fetal monitoring is done to check the baby’s heart rate and well-being.
Managing Pain After Surgery
Pain management after surgery is crucial to a comfortable recovery. Your doctor will provide you with pain medication and discuss the different options available.
- Medication: Painkillers, both over-the-counter and prescription, can help manage post-surgery pain.
- Ice packs: Applying ice packs to the surgical site can help reduce swelling and pain.
- Massage: Gentle massage therapy around the surgical site can aid in pain relief and relaxation.
Tips for a Smoother Recovery
- Rest: Allow your body to rest and recover. Avoid strenuous activities and get plenty of sleep.
- Hydration: Drink plenty of fluids to stay hydrated, which is essential for healing.
- Wound care: Follow your doctor’s instructions carefully regarding wound care.
- Support: Having a supportive partner, family, or friends during recovery can be invaluable.
Postpartum Care and Resources
Postpartum care after a Cesarean delivery involves regular checkups with your doctor to monitor your recovery. It’s also important to seek support services if needed.
- Postpartum checkups: Schedule regular checkups to ensure your recovery is progressing as expected.
- Lactation consultants: If you’re planning to breastfeed, a lactation consultant can help you overcome any challenges.
- Support groups: Joining a support group can provide a sense of community and shared experiences with other mothers who’ve had Cesarean deliveries.
- Home health aides: If you need additional assistance with childcare or household chores, a home health aide can provide support.
Emotional Preparation and Support
Preparing for a Cesarean delivery involves not only physical preparation but also emotional readiness. Acknowledge that you might experience a range of emotions, from disappointment to anxiety, and seek support to manage these feelings.
Addressing Emotions
- Disappointment: It’s common to feel disappointed if your birth plan changes, and you’re expecting a vaginal delivery but need a Cesarean instead.
- Anxiety: The thought of surgery and recovery can be anxiety-provoking.
- Sadness: It’s natural to feel a sense of sadness if you’re not experiencing a vaginal birth as you envisioned.
Building a Strong Support System
Having a strong support network can be incredibly helpful during this time.
- Partner: Your partner can be a source of emotional support and practical assistance.
- Family and friends: Family and friends can offer emotional support, help with childcare, and assist with household tasks.
- Support groups: Joining a support group can provide a sense of community with other mothers who understand your experiences.
Creating a Positive Mindset
Focus on the positive aspects of your situation. Remember that you’re bringing a new life into the world, and that’s a celebration worth cherishing.
- Focus on the health of your baby: Your priority is the health and well-being of your child.
- Celebrate the miracle of birth: Embrace the joy of becoming a parent.
- Seek professional help if needed: A therapist can provide guidance and support for managing emotional challenges.
Managing Expectations
It’s important to manage expectations about recovery time and physical limitations.
- Recovery takes time: Allow yourself time to heal and adjust to motherhood.
- Physical limitations: You might experience some limitations in your daily activities during the initial weeks of recovery.
- Patience is key: Be patient with yourself as you navigate this new phase of your life.
Breastfeeding After a Cesarean Delivery
Many women wonder if they can still breastfeed after a Cesarean delivery. The good news is that yes, breastfeeding is possible!
Breastfeeding Challenges and Strategies
- Early skin-to-skin contact: Immediately after delivery, if possible, ask for skin-to-skin contact with your baby to promote bonding and facilitate breastfeeding.
- Proper latch: It’s important to have a proper latch to ensure your baby is feeding effectively.
- Lactation consultants: A lactation consultant can help you overcome any challenges with latch, milk supply, or breastfeeding positions.
- Support groups: Joining a breastfeeding support group can provide valuable information, tips, and encouragement.
Alternatives to Breastfeeding
If breastfeeding doesn’t work for you, there are alternative feeding methods.
- Formula feeding: Formula feeding is a safe and healthy alternative to breastfeeding.
- Donor milk: Donor milk is pasteurized milk from screened mothers who have chosen to donate.
Questions to Ask Your Healthcare Provider
It’s crucial to talk to your doctor about any concerns you have about a Cesarean delivery. Here are some questions you can ask:
- What are the reasons for recommending a Cesarean delivery?
- What are the different anesthesia options available?
- What is the expected recovery time after a Cesarean delivery?
- How will pain be managed after surgery?
- What are the potential risks and complications of a Cesarean delivery?
- What support services are available after delivery?
- Can I still breastfeed after a Cesarean delivery?
- What resources are available for postpartum care and support?
Conclusion
While preparing for a Cesarean delivery can be challenging, it’s essential to remember that you’re not alone. It’s okay to ask for help and seek support. Your health and well-being are paramount, and there are resources available to guide you through this journey. To learn more about preparing for a Cesarean delivery, visit kienthucsannhi.com and share your experiences in the comments below.
FAQ:
What are the common types of anesthesia used for Cesarean deliveries?
Cesarean deliveries typically involve either a spinal block or an epidural. A spinal block is a single injection that numbs the lower half of the body, while an epidural is a continuous infusion of medication that provides pain relief throughout the procedure.
What are the most important things to remember about pain management after a Cesarean delivery?
Pain management after a Cesarean delivery is crucial for a comfortable recovery. Your doctor will discuss various methods to help you manage pain effectively. It’s essential to follow their instructions carefully and not hesitate to ask for additional pain relief if needed.
What are some tips for managing emotions after a Cesarean delivery?
Emotional well-being is essential for a healthy recovery after a Cesarean delivery. It’s normal to experience a range of emotions, including disappointment, anxiety, and sadness. It’s vital to acknowledge and process these emotions, seeking support from loved ones, a therapist, or support groups. Remember that you’re not alone, and it’s okay to reach out for help.
What are some resources available for postpartum care and support after a Cesarean delivery?
After a Cesarean delivery, you’ll need ongoing postpartum care to monitor your recovery. Several resources are available to help you navigate this transition.
- Home health aides: These professionals can provide assistance with childcare and household tasks, reducing your stress and allowing you to focus on healing.
- Support groups: Joining a support group connects you with other mothers who have had similar experiences and can offer valuable advice, support, and understanding.
- Lactation consultants: These specialists can assist with any challenges you might face with breastfeeding after a Cesarean delivery.
- Therapists: A therapist can provide emotional support and help you manage any postpartum mood changes.
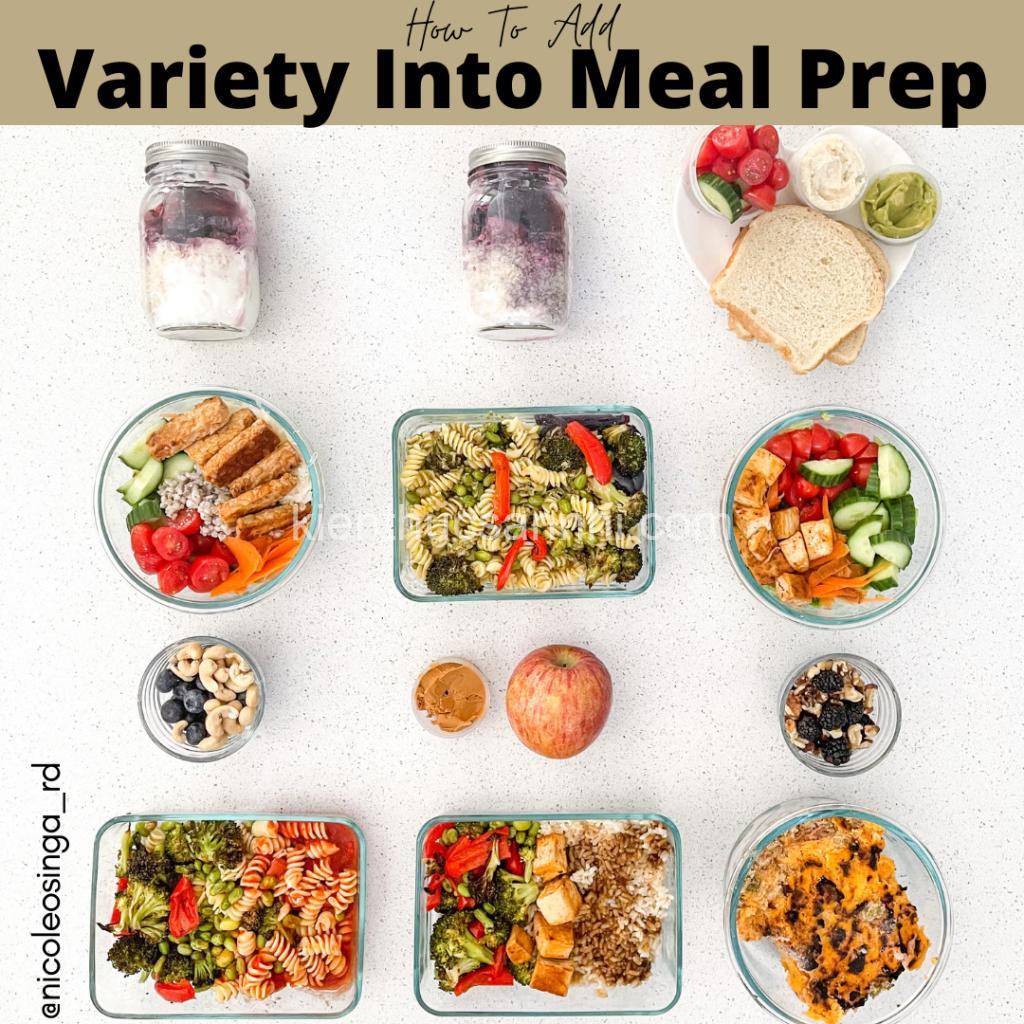
Are there any specific foods to avoid after a Cesarean delivery?
While your doctor will likely advise you on dietary restrictions, some general guidelines include:
- Avoiding foods that cause gas: Foods like beans, broccoli, and cabbage can lead to gas and discomfort.
- Limiting caffeine and alcohol: These can interfere with healing and cause dehydration.
- Eating plenty of fiber: Fiber-rich foods can help prevent constipation, a common concern after surgery.
EAVs:
- Cesarean Delivery | Type | Planned/Unplanned
- Cesarean Delivery | Anesthesia | Spinal/Epidural
- Pregnancy | Trimester | Third
- Recovery | Duration | 6-8 weeks
- Pain Management | Method | Medication/Ice Packs/Massage
- Breastfeeding | Challenges | Latch Difficulty/Milk Supply
- Emotional Support | Source | Partner/Family/Friends/Therapist
- Physical Support | Type | Assistance with Baby Care/Housework
- Medical Professionals | Role | Obstetrician/Nurse/Lactation Consultant
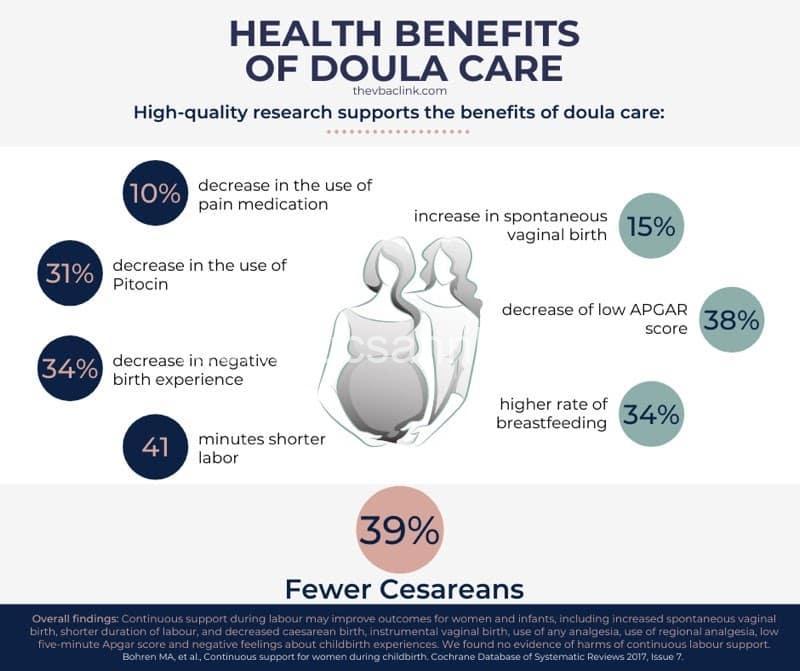
- Postpartum Care | Services | Home Health Aide/Doula/Support Groups
- Cesarean Delivery | Risks | Infection/Bleeding/Blood Clots
- Cesarean Delivery | Benefits | Safe Delivery for Mother/Baby
- Pregnancy | Complications | Premature Labor/Gestational Diabetes
- Recovery | Activities | Rest/Walking/Light Exercise
- Pain Management | Effectiveness | Varies by Individual
- Breastfeeding | Success Rate | Varies by Individual
- Emotional Support | Effectiveness | Varies by Individual
- Physical Support | Impact | Reduces Stress/Improves Recovery
- Medical Professionals | Expertise | Cesarean Delivery/Postpartum Care
- Postpartum Care | Availability | Varies by Location/Insurance
EREs:
- Cesarean Delivery | Performed by | Surgeon
- Pregnancy | Managed by | Obstetrician
- Recovery | Affected by | Anesthesia
- Pain Management | Provided by | Nurse/Doctor
- Breastfeeding | Assisted by | Lactation Consultant
- Emotional Support | Provided by | Partner/Family/Friends
- Physical Support | Provided by | Partner/Family/Friends
- Medical Professionals | Offer | Advice and Guidance
- Postpartum Care | Includes | Counseling/Support Groups
- Cesarean Delivery | Followed by | Recovery Period
- Pregnancy | Results in | Delivery
- Recovery | Facilitated by | Rest and Nutrition
- Pain Management | Reduces | Discomfort
- Breastfeeding | Benefits | Baby’s Health/Mother’s Recovery
- Emotional Support | Improves | Mental Well-being
- Physical Support | Reduces | Fatigue/Stress
- Medical Professionals | Provide | Medical Expertise
- Postpartum Care | Enhances | Overall Recovery
- Cesarean Delivery | Can cause | Physical Limitations
- Pregnancy | Can lead to | Postpartum Depression
Semantic Triples:
- Cesarean Delivery | is a | Surgical Procedure
- Pregnant Woman | undergoes | Cesarean Delivery
- Cesarean Delivery | requires | Anesthesia
- Recovery | follows | Cesarean Delivery
- Pain Management | helps with | Post-Surgery Discomfort
- Breastfeeding | is possible | After Cesarean Delivery
- Emotional Support | is important for | Postpartum Adjustment
- Physical Support | aids in | Recovery Process
- Medical Professionals | provide | Guidance and Care
- Postpartum Care | includes | Physical and Emotional Support
- Cesarean Delivery | can be | Planned or Unplanned
- Pregnancy | can have | Complications
- Recovery | takes time | to heal
- Pain Management | can use | Medication or Alternative Methods
- Breastfeeding | can be | Challenging
- Emotional Support | can come from | Various Sources
- Physical Support | can be | Provided by Family or Friends
- Medical Professionals | have | Specialized Knowledge
- Postpartum Care | is available | Through Various Programs
- Cesarean Delivery | can impact | Postpartum Recovery